

A 6-year-old boy is referred to the Epilepsy Center where he is first seen by a pediatric neurologist/epileptologist. The patient has a 4-year history of recurrent uncontrolled seizures of undetermined etiology. His seizures consist of daily episodes of stiffening and jerking of the extremities lasting for 30-60 seconds. Despite taking a combination of 3 antiepileptic medications at high doses he continues to experience multiple (up to 10) seizures per day. Several previous trials of antiepileptic medications have failed to control the seizures. The patient’s cognitive and social development has been normal, but his quality of life is considerably compromised due to his daily seizures and the side effects accompanying his high doses of antiepileptic medications.
The patient is admitted to the pediatric epilepsy monitoring unit (EMU) for a 5-day video-electroencephalography (video-EEG) evaluation in order to capture and characterize his seizures. To investigate whether the patient could benefit from epilepsy surgery, i.e. surgical resection of the focus giving rise to his seizures, this is the first step. The video-EEG suggested that the seizures were arising from the left side of the brain, but unfortunately did not provide further localizing information. High resolution magnetic resonance imaging (MRI) of the brain did not reveal any underlying structural abnormalities. Additional noninvasive tests including ictal SPECT (Single Photon Emission Computerized Tomography) and interictal FDG-PET (Fluoro-Deoxy-Glucose Positron Emission Tomography) were not helpful in pinpointing the seizure focus. Despite the use of these various diagnostic tests the localization of the seizure focus remained unclear, and therefore the patient was considered to be an unfavorable candidate for resective epilepsy surgery. The only alternative at this time was to continue several antiepileptic medications with no immediate prospect for improvement in his seizures and/or quality of life.
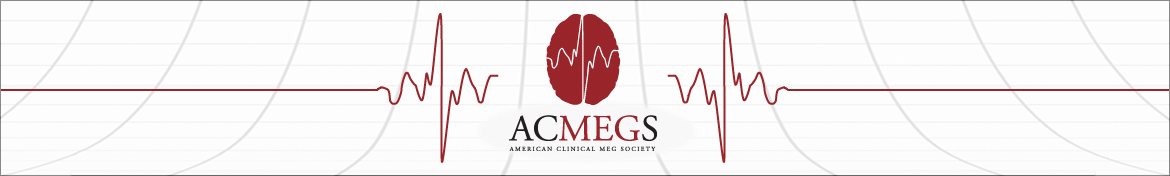
The patient’s seizures have continued unabated, occurring on average 4-5 times per day. The boy is now 10 years and his local neurologist again asks the pediatric epileptologist for re-evaluation. A repeat MRI is arranged (with higher resolution) and an MEG. The MRI is again considered to be within normal limits. The MEG study, however, provided the epilepsy team with new, previously unavailable, localizing information as illustrated in Figures 1A & 1B. The study shows that the patient’s abnormal epileptic activity (spikes) originates from a restricted location within the posterior part of the left hemisphere in the deeper gray matter of the posterior insula and inferior parietal cortex.
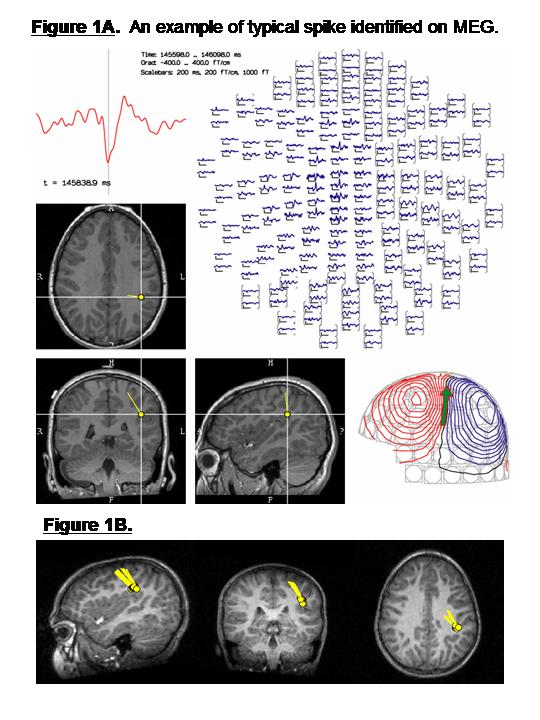
Figure 1. Based on measurements taken 1000 times per second from 306 MEG sensors arrayed around the head, the location of each individual spike can be accurately determined, using SECD (single equivalent current dipole modeling); localization of one spike is shown in Figure 1A. As illustrated in Figure 1B, all of the spikes are estimated to originate from within the same region of the posterior part of the patient’s brain, with a consistent and uniformly oriented magnetic field.
Armed with this new information the pediatric epileptologist arranges to bring the patient’s case for discussion in the multidisciplinary epilepsy patient management conference with his colleagues, a large group of more than 10 pediatric and adult epileptologists, along with clinical neurophysiologists, neuropsychologists, neuroradiologists and epilepsy neurosurgeons.
Prompted by the MEG data, the neuroradiologist focussed his attention to a particular area of interest on the patient’s MRI directed by the MEG findings. A very subtle and previously undetected MRI lesion of the cortex was identified within this same area (Figure 2).
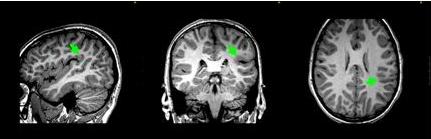
Figure 2. Careful scrutiny of the MRI in the region identified by the MEG revealed a subtle blurring of the grey-white border in the deep left parietal lobe.
The results of the patient’s MEG study and subsequent identification of a subtle lesion in the same region have changed the therapeutic outlook. With this clearly localizing information the patient can now be considered a candidate for epilepsy surgery. Given the intractable nature of the patient’s seizures the uniform opinion of the physicians participating in the patient management conference was that this patient should be referred to the epilepsy neurosurgery team. The neurosurgeon proceeded with implantation of intracranial electrodes to further define the extent of the seizure focus and, by mapping the patient’s language and sensory areas, its relationship to neighboring functional brain tissue. Placement of intracranial electrodes was again guided by the results of the MEG study and MRI findings. The results of the invasive evaluation performed by the neurosurgeon and a group of subspecialty-trained neurophysiologists and epileptologists confirmed that the area defined by the MEG was indeed harboring the seizure focus in this patient. Based on the results of the MEG and subsequent invasive evaluation with intracranial electrodes the neurosurgeon was now able to perform a limited resection of the seizure focus sparing surrounding functional areas of the brain. As illustrated in Figure 3 the area that was removed, which appears as a dark void on the patient’s postoperative MRI, corresponded exactly to the region that was first highlighted by the MEG.
Figure 3. MRI obtained after epilepsy surgery; showing the resected tissue as a dark spot. The location of this resection can be compared with the epileptogenic region first identified by MEG in figure 1 and then detected on MRI in Figure 2.
The patient returns for a routine follow-up visit with the pediatric epileptologist and the neurosurgeon 6 months after surgical resection of the seizure focus. He has not experienced any seizures since the surgery. He is doing well in school and attending regular classes. The epileptologist has been able to reduce the number and doses of his antiepileptic medications.
The patient is now 13 years old and has been seizure free for more than 1.5 years following epilepsy surgery.
MEG recordings were crucial in identifying the target in this patient and allowing him to be treated with successful epilepsy surgery.